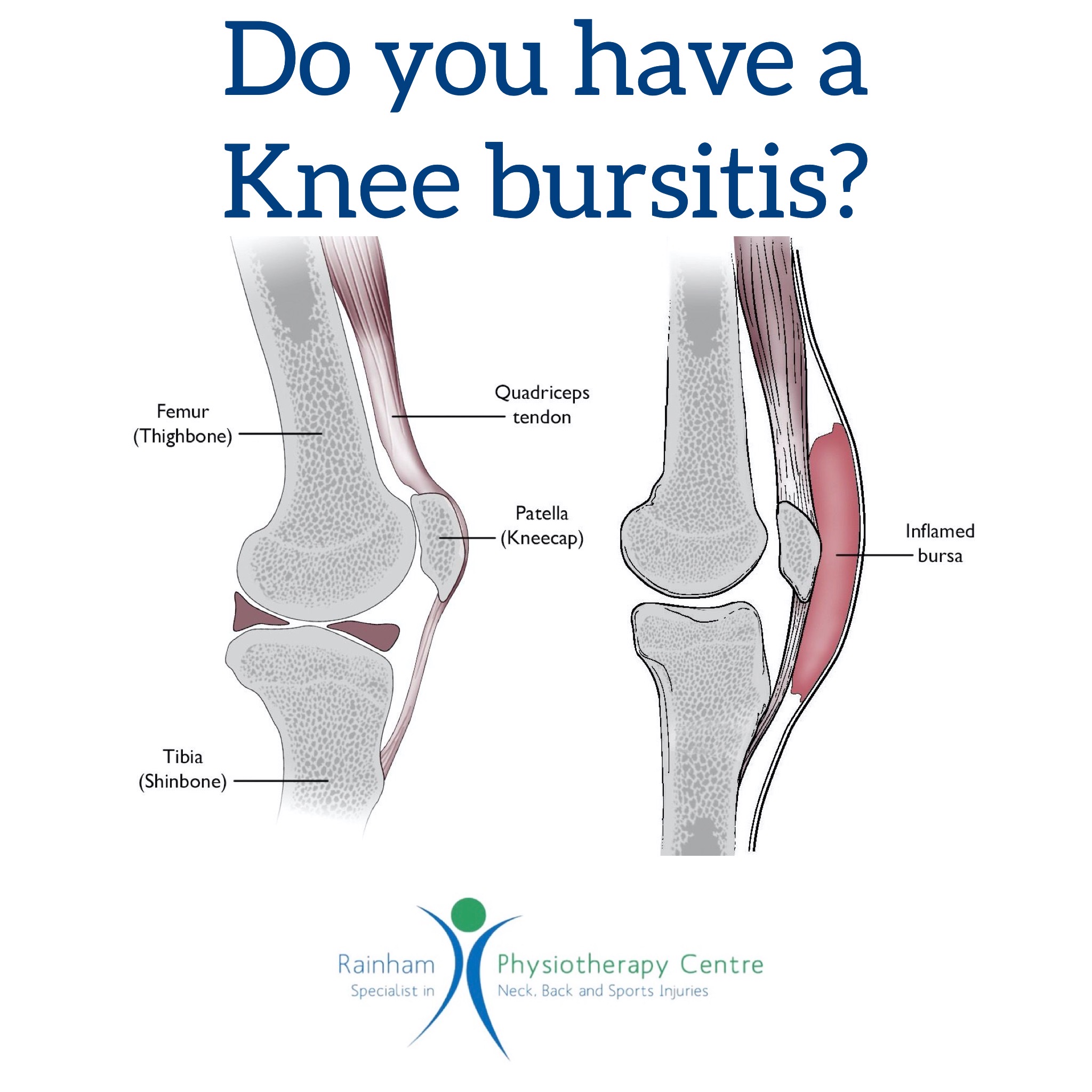
Do you have a knee bursitis?
Knee bursitis is inflammation of a small fluid-filled sac (bursa) near your knee joint. Bursae reduce friction and cushion pressure points between your bones and the tendons, muscles, and skin near your joints.
Knee bursitis symptoms vary, depending on which bursa is affected and what’s causing the inflammation.
In general, the affected portion of your knee might feel warm, tender and swollen when you put pressure on it. You might also feel pain when you move or even at rest.
A hit to the knee can cause symptoms to appear rapidly. But most cases of knee bursitis result from friction and irritation so symptoms usually begin gradually and worsen over time.
Causes
Knee bursitis can be caused by:
* Frequent and sustained pressure, such as from kneeling, especially on hard surfaces
* Overuse or strenuous activity
* A direct hit to your knee
* Bacterial infection of the bursa
* Complications from arthritis or gout in your knee
Therapy
Physiotherapists can help you improve flexibility and strengthen muscles. This therapy might alleviate pain and reduce your risk of recurring episodes of knee bursitis. Protective knee braces might help if you can’t avoid kneeling, and compressive knee sleeves can help reduce swelling.
More-invasive treatments for knee bursitis treatment include:
* Corticosteroid injection. If the bursitis is persistent and not responding to basic treatments, your doctor might inject a corticosteroid drug into an affected bursa to reduce inflammation. The inflammation usually subsides rapidly, but you might have pain and swelling from the injection for a couple of days.
* Aspiration. Your doctor might aspirate a bursa to reduce excess fluid and treat inflammation. He or she will insert a needle into the affected bursa and draw fluid into the syringe. Aspiration might cause short-term pain and swelling, and you might need to wear a knee immobiliser for a short period.
* Surgery. If you have severe chronic or recurrent bursitis and don’t respond to other treatments, your doctor might recommend surgery to remove the bursa.
Call us at Rainham Physiotherapy Centre on 01634 377638 to book in if you feel you may be suffering from this condition or on any issues you have.